Fall prevention is a critical aspect of healthcare that is aimed at reducing the incidence of falls among patients. According to the Centers for Disease Control and Prevention (CDC), falls are a significant public health issue and are responsible for about 3 million emergency department visits annually in the United States alone. Additionally, one in four elderly adults experience falls each year, and falls are the leading cause of injury-related deaths among those aged 65 and older.
Some refrain from using the term “fall” especially when an injury has been linked to the incident. The Centers for Medicare and Medicaid Services (CMS) defines a fall as an event that results in a person unintentionally coming to the ground or a lower level and other than because of a medical condition or external force (CMS, 2020) The definition includes falls with and without injuries.
Assessing for fall risk is crucial in identifying patients at risk. This measure is a first line approach in fall prevention and is the initial key element in preventing injuries associated with falls. Failure to identify patients at high risk of falling can result in serious injuries, such as fractures, head injuries, and dislocations, which can lead to long-term disability or death. Additionally, fall-related injuries can lead to increased healthcare costs, prolonged hospital stays, and decreased quality of life. Healthcare providers can also face legal liabilities should there be injuries because of failures to assess a patient’s fall risk and failure to implement a plan of care to prevent avoidable falls.
Assessment tools for fall risk are designed to help healthcare providers:
- identify those who are at risk of falls.
- Identify the factors which places them at risk for falls.
- Institute interventions that can reduce the risk for falls.
There are several fall risk assessment tools that maybe used to evaluate those at risk for falls. Though assessment tools for fall risk are being discussed, it is significant to note that in addition to the tool, the evaluator should use the clinical evaluation and their clinical judgement in determining the patient’s risk for falls. Three commonly used assessment tools for fall risk are discussed in this writing.
Assessment Tool #1: The Morse Fall Scale
The Morse Fall Scale is a widely used fall risk assessment tool. The Morse Fall Scale was created in 1989; it is used widely in acute care settings, both in the hospital and long-term care inpatient settings. A strength of the tool is its ease of use and interpretation, even for healthcare providers who are not specialized in fall prevention. Though its effectiveness has been validated in several studies, some critics argue that risk factors such as medication use, or environmental factors are not considered.
The scale uses six items to assess a patient’s fall risk:
- History of falling
- Secondary diagnosis
- Ambulatory aid
- Intravenous therapy
- Gait
- Mental status
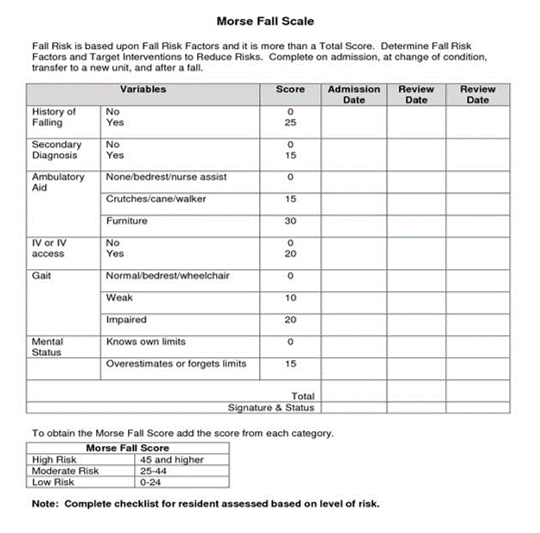
Each item is scored from 0 to 4, with a total score ranging from 0 to 125. The higher the score, the higher the risk of falling. A score of 0-24 indicates a low risk of falling, a score of 25-44 indicates a moderate risk of falling, and a score of 45 or higher indicates a high risk of falling.
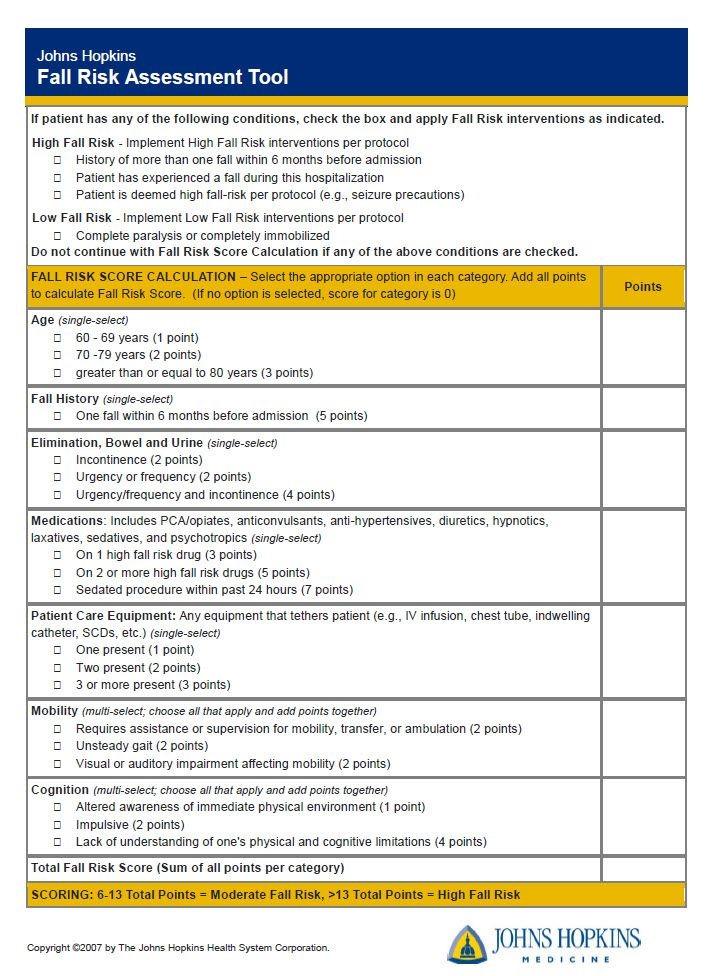
Assessment Tool # 2: The Johns Hopkins Fall Risk Assessment Tool (JHFRAT) was developed by nurses at the John Hopkins Hospital. It is evidence-based, and it is highly effective “when combined with a comprehensive protocol and fall prevention products and technologies.” The assessment tool is part of a toolkit that includes a purchased licensure to use the JHFRAT, The Johns Hopkins Fall Prevention guidelines by risk category, and training.
The tool consists of seven variables that are scored based on the patient’s history and current condition. The variables include:
- Age
- Cognitive status
- Fall history
- Gait and balance
- Mobility
- Sensory deficits
- Urinary incontinence
Points are assigned to each variable, with a total possible score ranging from 0 to 20. A higher score indicates a greater risk of falling. The JHFRAT is easy to administer and interpret, and it has been shown to have good predictive validity. (Young and et al. 2022)
“The Johns Hopkins Fall Risk Assessment Tool is the intellectual property of the Johns Hopkins Healthcare System and may not be used without a license.” The image of the JHFRAT in this writing is being used with permission from the institution.
Assessment Tool #3: The Hendrich II Fall Risk Assessment
The Hendrich II Fall Risk Assessment was created through research of completed physical examinations of fall and non-fall patients using standardized assessment tools; eight risk factors were found necessary to prevent falls. Findings indicated that age and a history of falling were not independent risk factors for falling. The Hendrich II Fall Risk Assessment tool can be used in many clinical settings: adult acute care, ambulatory, assisted living, and long-term care. A purchased licensure is required to use the fall risk model. The model includes training and interventions based upon the assessed risk factors.
The strength of the Henrich II Fall Risk tool is its brevity and its focus on specific areas of risk, rather than on a general risk score.
These are the eight (8) risk factors that were identified through research to predict falls:
- Confusion/Disorientation/Impulsivity
- Symptomatic Depression
- Altered Elimination
- Dizziness/vertigo
- Gender (male)
- Administered Antiepileptics
- Administered Benzodiazepines, opioids
- Get-up-an-go Test: Rising from chair
Some Frequently Asked Questions
How do you know if a fall risk assessment has been conducted?
Preventing falls is one of the quality and safety measures in healthcare. As a part of that initiative, a fall risk assessment is to be conducted on entry in the facility (emergency room) and on admission to the facility. Additionally, fall risk assessments are done if a change in condition and quarterly in the long-term care settings. If a fall risk assessment has been conducted, it will be recorded in the patient’s medical records. The healthcare provider responsible for conducting the assessment will document the results of the evaluation. As there are many fall risk assessment tools and the tool used is facility specific, the name of the specific tool used may or may not be listed.
How long does it take to administer a fall risk assessment?
The administration of a fall risk assessment can vary depending on the tool used, the complexity of the patient’s medical history, and the patient’s overall health status. Typically, a fall risk assessment can take anywhere from 5 to 30 minutes, depending on the assessment tool used and the patient’s and cognitive function and level of mobility. Read about fall prevention in medical facilities here.
How can a Legal Nurse Consultant (LNC) decipher a fall risk assessment?
Based upon the diagnosis of the patient, the documented physical assessment of the patient, and the standards of care, the LNC can determine whether appropriate clinical assessment was utilized in evaluating the risk factors for the patient.
How can a Legal Nurse Consultant (LNC) benefit an attorney in a fall case?
- Review and analyze the medical records.
- Determine whether a fall risk assessment was done
- Evaluate the fall risk assessment relevancy to the clinical assessment
- Determine whether a plan of care for fall prevention was developed
- Analyze the interventions of the plan of care appropriateness to the risk factors for a fall
- Review the medical records for implementation of the plan of care
- Determine whether a deviation in the standards of care in providing the patient care
- Determine whether the deviation in the standards of care lead to the fall
The attorney needs experts, how can the Legal Nurse Consultant help?
The LNC can provide expert opinions on the care of another health care provider of a similar background and of the same medical community.
The LNC expert can opine on:
- The standard of care related to the fall risk assessment
- Identification of the fall risk factors
- Fall Prevention plan of care
- Implementation of the interventions for fall prevention
- Deviations, if any, in the standards of care
- Relationship of the deviation in the standards of care, if any, to the fall
The LNC can help locate additional experts, if needed.
Depositions and trial will be scheduled, how can the LNC help?
- Assist with preparation of depositions questions.
- Create exhibits and presentations
- Prepare demonstrations
In conclusion, Falls and associated injuries can impact any age groups. Being especially vulnerable, it is crucial to assess the elderly individuals for factors that may cause them to be at risk for fall associated injury. Many assessment tools for fall risk are available; among the most used are The Morse Fall Scale, Johns Hopkins Fall Assessment Tool, and the Hendrich II Fall Risk Model. Regardless of the assessment tool used, the clinical presentation of the patient should be considered in evaluating the patient for fall risk factors.
Once factors are identified that cause patients to be at risk for falls, the next step for the healthcare team is to create a plan of care to address those modifiable factors. A comprehensive fall prevention program can help reduce the likelihood of falls and related injuries, improving patient outcomes and reducing healthcare costs. Early identification of fall risk factors can also help healthcare providers make informed decisions about patient care, including the need for additional care, rehabilitation, or home health services
References:
Centers for Medicare and Medicaid Services (2020). CARE-2 (NQF 0101): Falls: Screening for Future Fall Risk 2020. Retrieved from
“Hendrich II”. https://hendrichfallriskmodel.com/
“Johns Hopkins Fall Risk Assessment Tool”. https://www.hopkinsmedicine.org/institute_nursing/_docs/JHFRAT/9_2_16_JHFRAT%20Flyer.3.pdf
Morse, J. M., Morse, R. M., & Tylko, S. J. (1989). Morse Fall Scale (MFS) [Database record]. APA PsycTests. https://doi.org/10.1037/t24759-000
Young, Ju Kim, Kyoung-Ok Choi , Suk Hyun Cho Seok ,Jung Kim (2022). (Validity of the Morse Fall Scale and the Johns Hopkins Fall Risk Assessment Tool for fall risk assessment in an acute care setting. https://pubmed.ncbi.nlm.nih.gov/34964175/
“Older Adult Fall Prevention”. https://www.cdc.gov/falls/index.html